Topic Tags:
If you’re looking for official hospital cleaning procedures and methods in Australia, the national reference points are the NSQHS Standards and the Australian Guidelines for the Prevention and Control of Infection in Healthcare. Together, they require hospitals to operate a risk‑based environmental cleaning program, use TGA‑listed hospital‑grade products, and prove effectiveness through training, supervision and audit.
Top 3 takeaways from the guide:
- Risk-based and documented: Every area has a defined method, frequency and responsible role; higher‑risk zones (e.g., isolation rooms, theatres) require more frequent cleaning and disinfection.
- Two pillars: Daily routine environmental cleaning (detergent first) and terminal cleaning (thorough clean plus disinfection after discharge/transfer or end of theatre list).
- Prove it works: Facilities must audit cleaning quality (visual checks plus objective methods), maintain records, and ensure staff are trained and competent.
1) National framework at a glance
- Governance: A designated manager (e.g., Environmental Services) oversees policies, schedules, training, and audits in partnership with Infection Prevention and Control (IPC).
- Products: Use TGA‑listed hospital‑grade disinfectants; prepare detergents/disinfectants to manufacturer instructions; never mix chemicals.
- Risk assessment: Classify areas (low, moderate, high risk) to set method + frequency. Prioritise high‑touch surfaces.
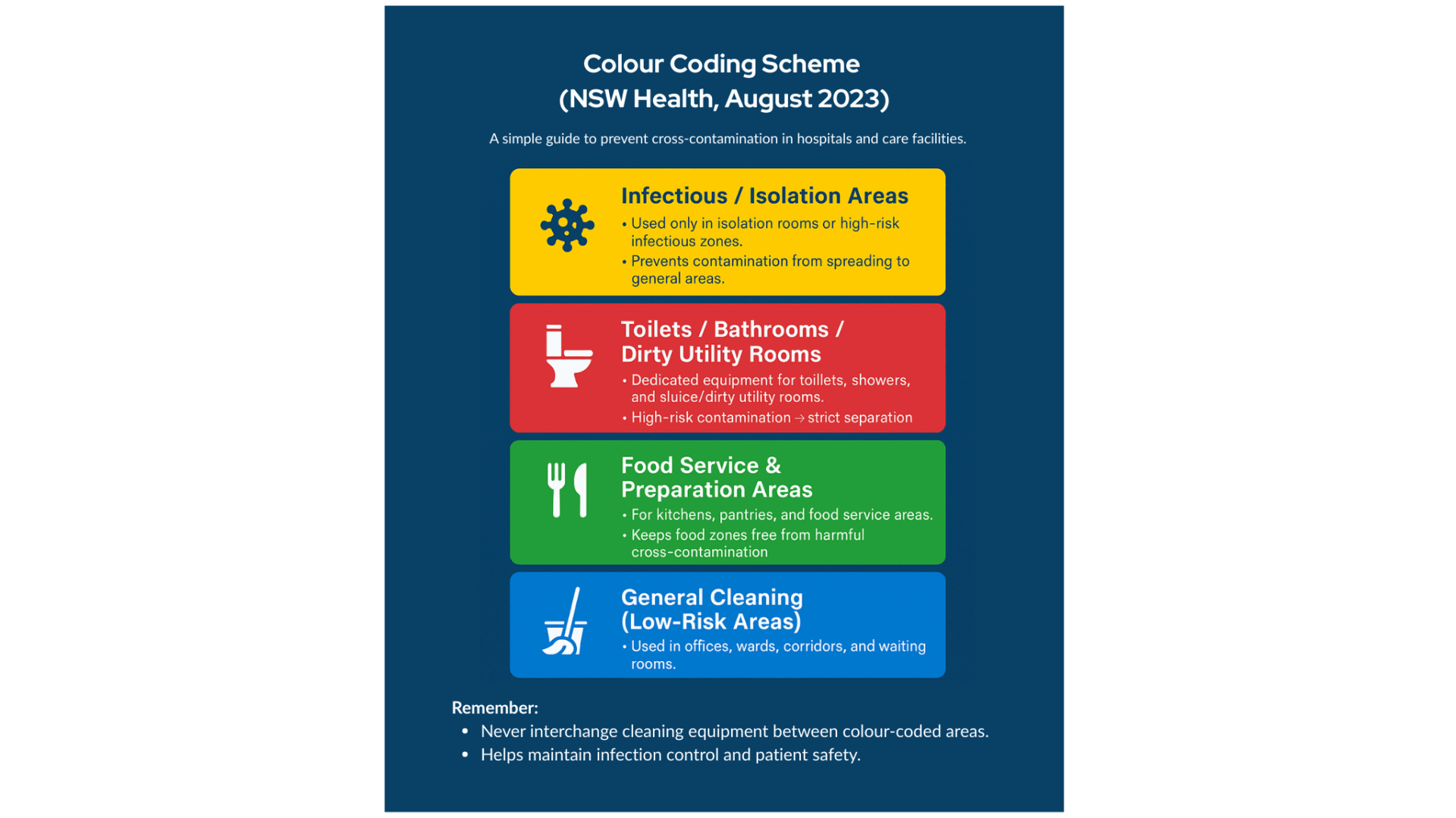
- Colour coding & equipment: Prevent cross‑contamination with colour‑coded cloths/mops; launder or dispose of items after each use.
2) Routine environmental cleaning — methods & frequencies
Purpose: Keep the environment visibly clean, reduce bioburden, and minimise transmission risk.
Method (how to clean)
- Preparation & PPE: Perform hand hygiene; don gloves (and other PPE if splash/chemical risk). Make a fresh detergent solution; assemble the colour‑coded gear.
- Order of work: Clean top → bottom and clean → dirty to prevent re‑contamination; use straight or “S‑pattern” strokes. Avoid dry dusting or spraying into the air; use damp wiping.
- Detergent first: Use a neutral detergent for general surface/floor cleaning. If the risk is elevated (e.g., outbreak, contact precautions), follow with disinfectant on high‑touch points.
- Equipment care: Replace cloths/mop heads between rooms; clean and dry buckets/tools after use.
Frequencies (typical baselines)
- High‑touch points (push plates, elevator call buttons, dispensers, light switches, door handles): clean at least daily and when soiled; more often in high‑risk zones.
- Patient rooms & bathrooms: Daily clean; bathrooms and toilets may require multiple checks/cleans per day.
- Clinical corridors/wards: Daily floors; spot clean spills immediately.
- Administrative/low‑risk areas: Daily or per schedule, with increased attention during outbreaks.
Responsibilities: Environmental services staff perform room, bathroom and common‑area cleaning. Clinical staff clean certain patient‑care equipment between uses, as defined in local policy.
3) Terminal cleaning after patient discharge/transfer
When: After a patient leaves a room (discharge/transfer), after transmission‑based precautions, and at the end of the day for operating theatres.
Goal: Thoroughly clean and disinfect every surface to reset the room for the next patient.
Step‑by‑step procedure:
- PPE & set‑up: Post area closed for cleaning if needed; don gloves and additional PPE (gown/mask/eye protection based on risk). Gather fresh supplies.
- Remove waste & linens: Bag all waste; remove used linen and curtains (send to laundry or dispose if single‑use). Remove disposable patient‑care items.
- Declutter & isolate equipment: Remove portable equipment for separate cleaning; ensure sharps are safely managed according to policy.
- Detergent clean — all surfaces: Methodically clean high to low and clean to dirty: bed, mattress (inspect), bedframe, call bell, rails, tables, chairs, monitors/IV poles, switches, handles, doors, walls if soiled, window ledges, and ensuite surfaces. Vacuum (HEPA) or damp‑mop floors.
- Disinfect: Apply hospital‑grade disinfectant (or 2‑in‑1 detergent/disinfectant) to all relevant surfaces with correct contact time. Give extra attention to high‑touch and bathroom fixtures.
- Reinstate room: After drying, remake bed with clean linen, hang clean curtains, restock supplies.
- Doff PPE & hand hygiene: Remove PPE safely; perform hand hygiene. Sign‑off using a terminal clean checklist/inspection.
4) Operating theatres and between‑case cleaning
- Between cases: Remove waste/linen; clean and disinfect the table, trolley tops, lights/handles, switches, and any contaminated surfaces; spot clean floor.
- End of list/daily: Conduct a terminal clean of the theatre and scrub/ancillary rooms, including full surface disinfection and wet mopping of floors; schedule periodic deep cleans for ceilings, vents and fixtures.
5) Auditing, monitoring and competency
- Audits: Use visual checks plus objective tools (e.g., fluorescent markers, ATP) on a risk‑based schedule. Track pass rates and remediate.
- Training & supervision: Induct and assess cleaners in IPC, chemical safety, colour coding, and method; refresh training regularly.
- Documentation: Maintain policies, area schedules, product lists/SDS, checklists, and audit records as evidence of compliance.
6) Product & safety notes
- Prepare solutions fresh; label and store chemicals safely.
- Do not mix detergents and disinfectants unless a combined product is specified.
- Maintain equipment (e.g., change mop heads; clean/dry buckets; service machines) to avoid cross‑contamination.

Partner with Namoli Healthcare for Expert Hospital Cleaning
At Namoli Healthcare, we specialise exclusively in healthcare cleaning. Our accredited teams follow Australian hospital cleaning standards, including routine environmental cleaning, terminal cleaning after patient discharge, and infection control audits.
Whether you manage a ward, theatre, or entire facility, NHC provides TGA-approved products, advanced equipment, and transparent auditing to ensure every clean meets the highest standards. Partner with us to achieve more than just a visibly clean hospital — achieve true clinical safety and peace of mind.
Related Posts
Topic Tags: Sapovirus is a common cause of acute gastroenteritis, particularly in young children and aged‑care settings. Although symptoms are…
Topic Tags: Effective infection control is central to resident safety in aged care, where close living environments, chronic illness, and…
Topic Tags: In healthcare environments, many pathogens spread through high-touch surfaces that look clean but still carry organic residue. Traditional…