-
Michael has been in the commercial cleaning and facilities management industry since 1991, bringing 34 years of hands-on and leadership experience. He has specialised in healthcare cleaning since 2005, applying 20 years of expertise in infection prevention and hygiene management. Over the past 20 years in senior management roles, Michael has successfully led operations, developed national compliance programs, and built high-performing teams across Australia’s healthcare sector.
View all posts
Topic Tags:
Published for World Hand Hygiene Day – 5th May
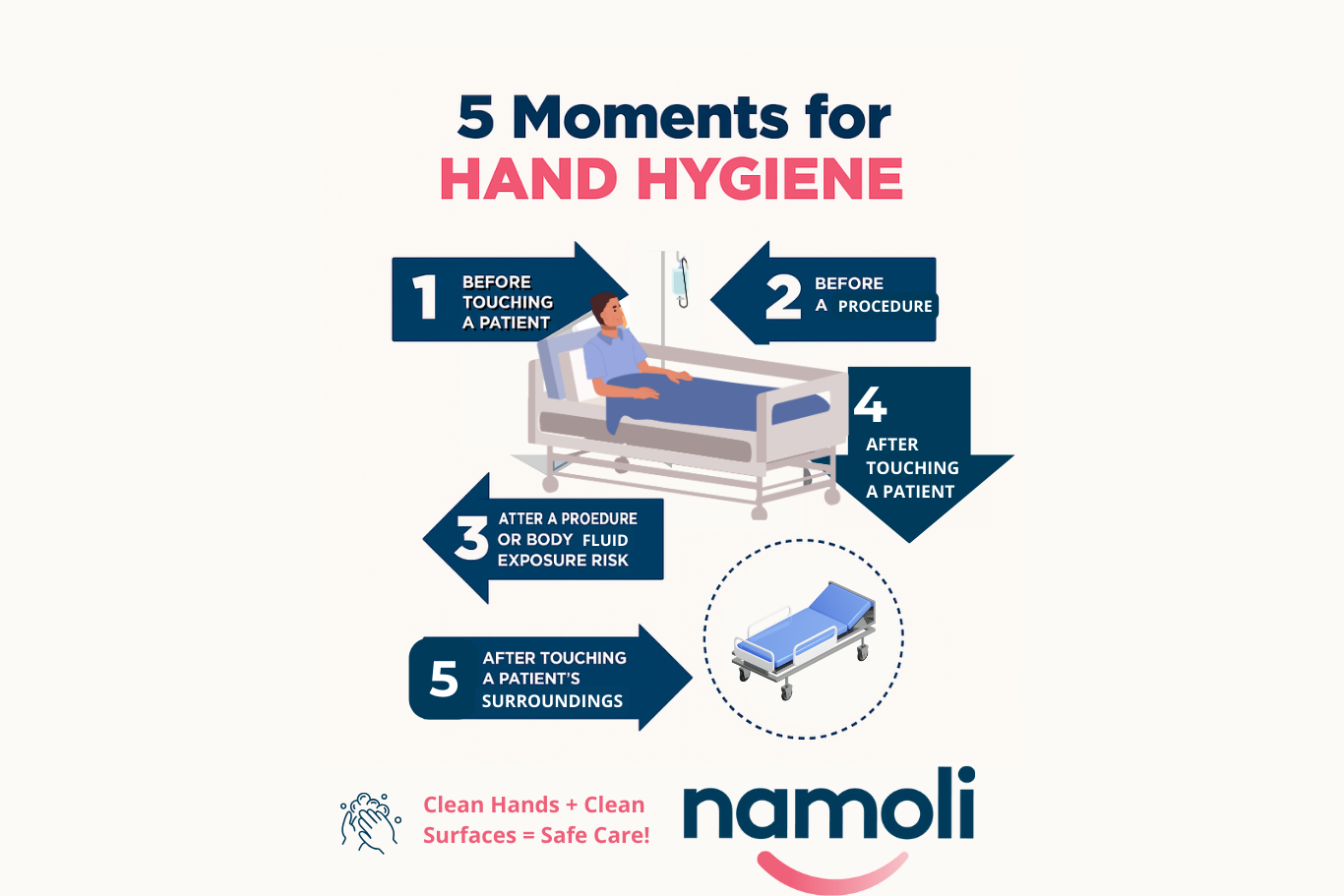
The WHO’s Five Moments for Hand Hygiene are critical in stopping the spread of infection. This article describes each moment and connects them to environmental touchpoints, illustrating how hands and surfaces work together in infection prevention.
Key Takeaways
- Before touching a patient and before a clean or aseptic procedure, hand hygiene protects patients from organisms on healthcare workers’ hands.
- After body fluid exposure and after touching a patient, hand hygiene prevents pathogens from spreading to other surfaces, equipment or people.
- After touching patient surroundings, disinfecting both hands and surfaces breaks the transmission cycle; high‑touch points must be cleaned to complement hand hygiene.
What Are the 5 Moments for Hand Hygiene?
The 5 Moments for Hand Hygiene, developed by the WHO and adopted in national guidelines across Australia, define the key times when healthcare workers should perform hand hygiene to protect themselves and their patients from healthcare-associated infections (HAIs).
Each moment isn’t just about hand hygiene, it’s about understanding the environment too. Here’s how surface contact plays a hidden but powerful role.
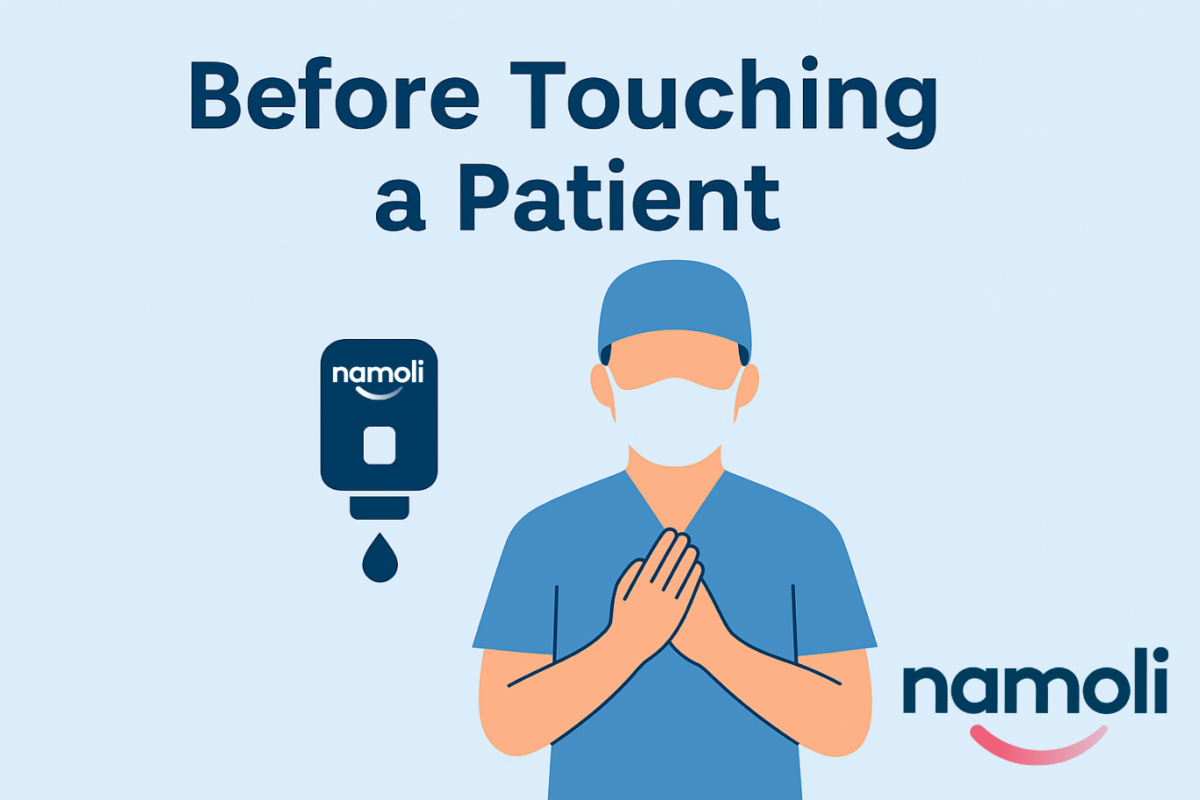
1. Before Touching a Patient
Why it matters:
You may carry microorganisms from shared spaces like reception counters, waiting room chairs, or even your own phone. Visitors and staff can unknowingly introduce these pathogens into patient areas.
Surface risk example:
Touching a visitor armrest, check-in touchscreen, or lift button before entering a patient room can transfer germs directly to the patient during contact.
Tip for teams:
Ensure high-traffic surfaces in entry and reception areas are disinfected frequently, and make hand sanitiser easily accessible for both staff and visitors.
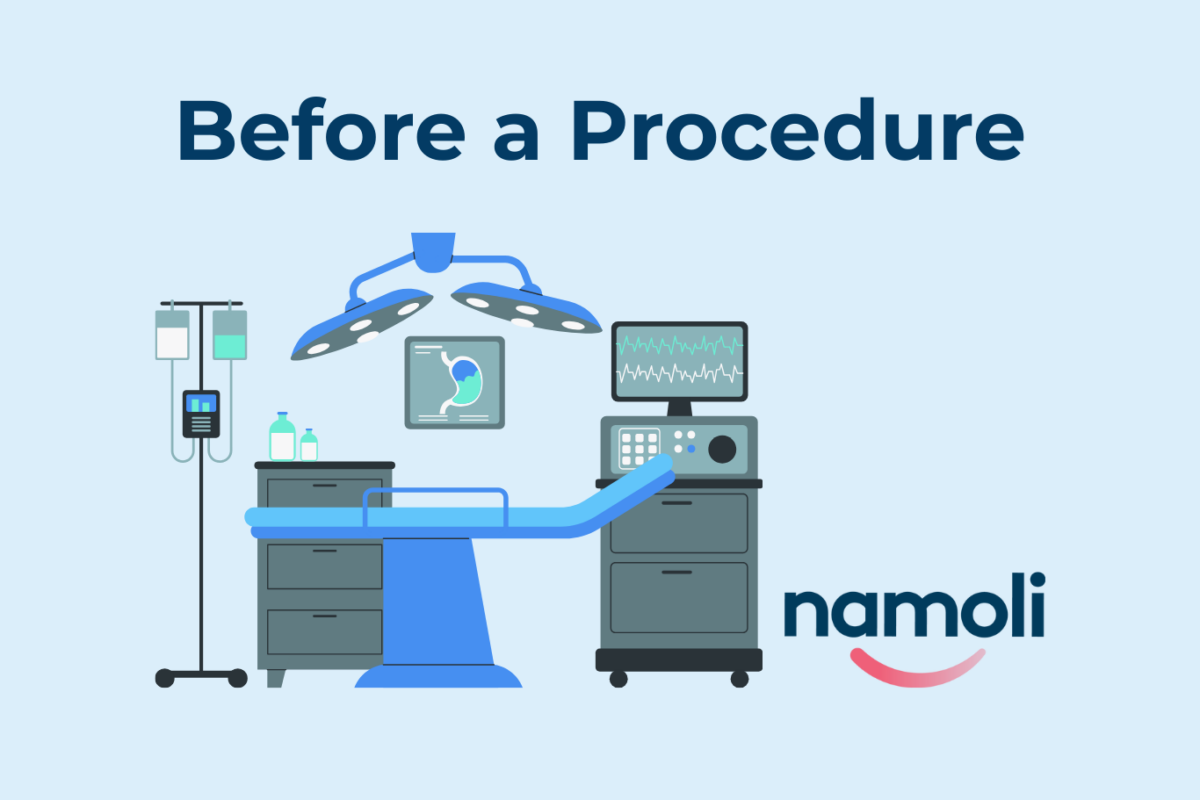
2. Before a Clean or Aseptic Procedure
Why it matters:
Even invisible germs on hands or surfaces can become dangerous when introduced into the body during procedures like dressing changes or wound care.
Surface risk example:
Touching curtain edges, nearby tray tables, or visitor-shared counters before a procedure may introduce contaminants to a sterile field.
Tip for teams:
Use TGA-approved disinfectants on all surfaces involved in procedures, and clean frequently touched items like over-bed tables, handles, and visitor seating before use.
3. After Body Fluid Exposure Risk
Why it matters:
Blood, saliva, and other body fluids pose a high risk for spreading infections—not just directly but via the surfaces they contact.
Surface risk example:
Splashes on examination bed rails, chair arms, or visitor-present areas that aren’t immediately cleaned can spread pathogens within the environment.
Tip for teams:
Pair hand hygiene with prompt surface disinfection after any exposure. Ensure cleaning protocols also extend to adjacent surfaces visitors may contact during or after a procedure.
4. After Touching a Patient
Why it matters:
Even with gloves, microorganisms can transfer to hands or nearby surfaces—and then spread to high-touch areas used by others.
Surface risk example:
After assisting a patient, staff may open doors, use workstation keyboards, or lean on visitor chairs—potentially contaminating shared environments.
Tip for teams:
Reinforce hygiene awareness not just at the point of care, but when transitioning between patients, spaces, or interacting with visitor zones.

5. After Touching a Patient’s Surroundings
Why it matters:
Surfaces near patients—like bedside tables, visitor chairs, or personal items—can be contaminated even if the patient shows no outward symptoms.
Surface risk example:
Adjusting the window blind, using the bedside handrail, or moving a visitor’s chair without cleaning or sanitising can propagate infections beyond the immediate patient space.
Tip for teams: Include visitor contact surfaces in touch point cleaning in your audit checklist and clean high-risk areas multiple times daily.

Why Are the 5 Moments So Important?
The 5 Moments of Hand Hygiene aren’t just a compliance checklist—they’re a behavioural framework grounded in infection control science. When combined with environmental cleaning best practices, they drastically reduce the risk of HAIs in both acute and primary care settings.
Evidence Behind Combined Hygiene Protocols
The link between hand hygiene and environmental cleaning it’s backed by science.
A growing body of research shows that when both protocols are followed together, the outcome is significantly more effective in reducing healthcare-associated infections (HAIs) than when either is used in isolation.
Key Research Insights:
- A 2022 systematic review of 26 studies on healthcare environmental hygiene (HEH) found that most interventions led to a reduction in patient colonisation or HAIs, particularly when cleaning was combined with hand hygiene strategies.
- An environmental cleaning bundle introduced in hospital settings showed a notable drop in vancomycin-resistant enterococci infections, underlining the role of thorough surface disinfection alongside routine hand hygiene【source: The Lancet ID†ScienceDirect】.
According to the World Health Organisation, hand hygiene alone can prevent up to 50% of avoidable infections during care delivery—highlighting its importance when paired with surface-level protocols
Bonus Download: Infographic – 5 Moments of Hand Hygiene

Partner With a Cleaning Provider That Understands Clinical Context
Namoli doesn’t just clean—we help healthcare teams stay compliant, reduce infection risks, and educate staff about hygiene touch points that matter most.
-
Michael has been in the commercial cleaning and facilities management industry since 1991, bringing 34 years of hands-on and leadership experience. He has specialised in healthcare cleaning since 2005, applying 20 years of expertise in infection prevention and hygiene management. Over the past 20 years in senior management roles, Michael has successfully led operations, developed national compliance programs, and built high-performing teams across Australia’s healthcare sector.
View all posts
Related Posts
-
Michael has been in the commercial cleaning and facilities management industry since 1991, bringing 34 years of hands-on and leadership experience. He has specialised in healthcare cleaning since 2005, applying 20 years of expertise in infection prevention and hygiene management. Over the past 20 years in senior management roles, Michael has successfully led operations, developed national compliance programs, and built high-performing teams across Australia’s healthcare sector.
Topic Tags: Effective infection control is central to resident safety in aged care, where close living environments, chronic illness, and…
-
Michael has been in the commercial cleaning and facilities management industry since 1991, bringing 34 years of hands-on and leadership experience. He has specialised in healthcare cleaning since 2005, applying 20 years of expertise in infection prevention and hygiene management. Over the past 20 years in senior management roles, Michael has successfully led operations, developed national compliance programs, and built high-performing teams across Australia’s healthcare sector.
-
Michael has been in the commercial cleaning and facilities management industry since 1991, bringing 34 years of hands-on and leadership experience. He has specialised in healthcare cleaning since 2005, applying 20 years of expertise in infection prevention and hygiene management. Over the past 20 years in senior management roles, Michael has successfully led operations, developed national compliance programs, and built high-performing teams across Australia’s healthcare sector.
Topic Tags: In healthcare environments, many pathogens spread through high-touch surfaces that look clean but still carry organic residue. Traditional…
-
Michael has been in the commercial cleaning and facilities management industry since 1991, bringing 34 years of hands-on and leadership experience. He has specialised in healthcare cleaning since 2005, applying 20 years of expertise in infection prevention and hygiene management. Over the past 20 years in senior management roles, Michael has successfully led operations, developed national compliance programs, and built high-performing teams across Australia’s healthcare sector.
-
Michael has been in the commercial cleaning and facilities management industry since 1991, bringing 34 years of hands-on and leadership experience. He has specialised in healthcare cleaning since 2005, applying 20 years of expertise in infection prevention and hygiene management. Over the past 20 years in senior management roles, Michael has successfully led operations, developed national compliance programs, and built high-performing teams across Australia’s healthcare sector.
Topic Tags: Maintaining a safe, clean environment in aged care facilities is essential for protecting residents, supporting staff, and meeting…
-
Michael has been in the commercial cleaning and facilities management industry since 1991, bringing 34 years of hands-on and leadership experience. He has specialised in healthcare cleaning since 2005, applying 20 years of expertise in infection prevention and hygiene management. Over the past 20 years in senior management roles, Michael has successfully led operations, developed national compliance programs, and built high-performing teams across Australia’s healthcare sector.