Topic Tags:
Published for World Hand Hygiene Day – 5th May
Healthcare‑associated infections are preventable—but they require diligence. This article explores the main routes of HAI transmission and explains how integrated hand hygiene, environmental cleaning and infection‑control protocols can break the chain of infection.
Key Takeaways
- HAIs spread through direct contact, contaminated surfaces and medical equipment; cleaning high‑touch areas and equipment disrupts transmission.
- Hand hygiene, proper PPE use and routine environmental disinfection are essential to reduce pathogens in clinical settings.
- Collaboration between clinical staff and cleaning teams, along with education and adherence to national guidelines, significantly reduces HAI rates.
A Day in the Life: Infection Control in Motion
At 7:30am, Claire, a nurse at a busy day surgery centre in Brisbane, starts her shift with a routine check on her patient list. Before she even touches her first patient, she uses alcohol-based hand rub and checks that the nearby blood pressure cuff has been properly wiped down by the cleaning team. It’s second nature now, but it wasn’t always this way.
“You don’t realise how many surfaces you touch between patients—monitors, call buttons, trolley handles,” Claire says. “Once we started paying attention, it changed everything.“
What Are Healthcare-Associated Infections (HAIs)?
HAIs are infections acquired by patients during their care in a healthcare setting that were not present at the time of admission. In Australia, tens of thousands of cases are recorded each year, and many are preventable with the right protocols.
Common HAIs include:
1. Urinary Tract Infection (CAUTI)
E.g., A patient in recovery with an indwelling catheter develops a UTI after the catheter was inserted without full aseptic technique.
2. Surgical Site Infection (SSI)
E.g., Following a routine knee replacement, a patient returns with redness and discharge around the incision due to poor wound care practices post-op.
3. Central Line-Associated Bloodstream Infection (CLABSI)
E.g., A cancer patient with a central venous catheter develops a bloodstream infection after repeated handling of the line without proper hand hygiene.
4. Ventilator-Associated Pneumonia (VAP)
E.g., A patient in ICU on mechanical ventilation contracts pneumonia after oral care routines are missed and suction equipment isn’t fully disinfected.
5. Clostridioides difficile Infection (C. diff)
E.g., An elderly patient receiving antibiotics develops severe diarrhoea after being exposed to C. diff spores on contaminated bathroom surfaces.6. Hospital-Acquired Pneumonia
E.g., A patient admitted for a non-respiratory issue develops pneumonia after spending several days in a shared room where high-touch surfaces weren’t regularly disinfected.

These infections increase costs and can have severe, sometimes fatal, consequences.
From Handwashing to High-Touch Zones: The Real Risk
While hand hygiene is rightly known as the single most important intervention to prevent HAIs, many infections occur indirectly—through contaminated surfaces shared by visitors, patients, and healthcare workers.
Think of how often people touch:
- Door handles in reception areas and patient rooms
- Light switches in shared spaces
- Armrests on waiting room chairs
- Touchscreens or check-in kiosks at entry points
- Lift buttons and handrails in hallways
- Shared keyboards and mouse devices at staff stations
- Countertops and pens at the reception desk

If just one of these touch points becomes a carrier of bacteria, the entire infection control ecosystem can be compromised, impacting staff and patients alike.Read more: More Than Just Hands: How Clean Surfaces Support Safe Care
Behaviour That Builds Barriers – Not Breaches
Preventing HAIs requires habitual, mindful hygiene that extends beyond just hand washing. It includes:
- Hand washing procedures using soap and water or alcohol-based rub before and after patient contact
- Disinfecting high-touch surfaces multiple times a day with TGA-approved products, especially in high-traffic visitor areas
- Correct use of PPE during procedures and patient interactions
- Documentation and surveillance to identify hotspots and act early
- Staff education and training on HAI prevention measures
- Early identification and isolation of symptomatic patients
By cleaning the surfaces that visitors and staff interact with most frequently, Namoli Healthcare plays a vital role in disrupting the chain of infection—creating safer environments for everyone.
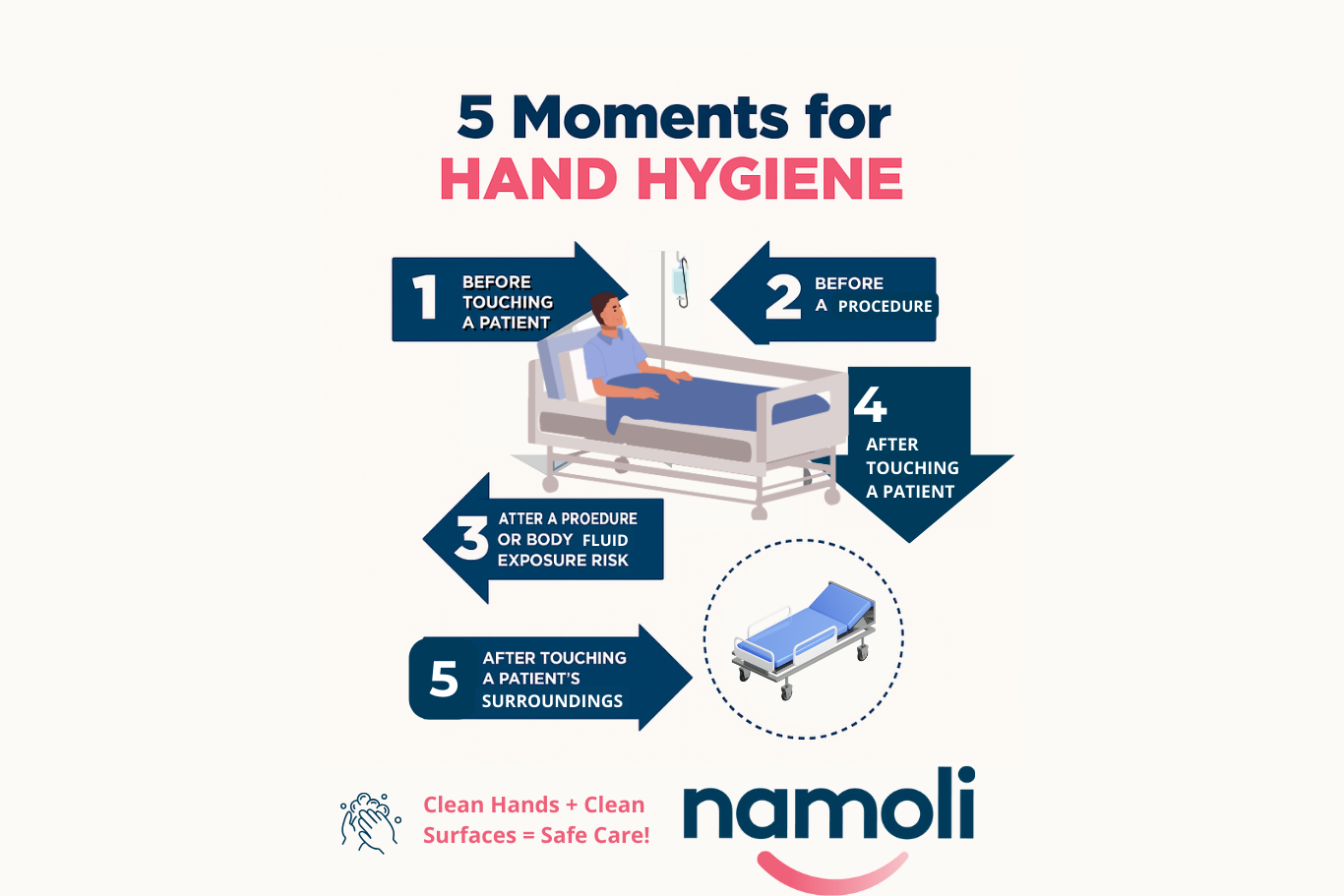
Read more: Five Moments for Hand Hygiene – And the Hidden Risk on Surfaces
Claire puts it simply:
“Hand hygiene and surface cleaning have to be a team effort. We rely on each other. One slip can undo a whole shift of good work.”
Programmes, Guidelines & the Role of Support Staff
Australia’s National Hand Hygiene Initiative, alongside international frameworks like the WHO’s 5 Moments for Hand Hygiene, provide a clear roadmap for HAI prevention. But guidelines alone aren’t enough.At Namoli Healthcare, we partner with day surgeries, medical centres, and pathology clinics to embed infection prevention protocols into the daily rhythm of care. From audit-ready cleaning programs to ongoing staff support, we ensure the environment is visibly clean and clinically safe.
Why This Matters More Than Ever
According to recent reviews:
- A systematic study of 26 environmental cleaning trials showed significant reductions in HAIs when protocols were combined with hand hygiene efforts.
- The most common cause of HAIs is bacterial transmission via hands and contaminated surfaces.
- In some Australian states, HAIs are the most frequent hospital-acquired complication.

From Hands to Handles: It’s a Shared Fight
Infection control isn’t one person’s job. It’s a coordinated defence—from clinical staff washing their hands to cleaning teams disinfecting chair arms, from procurement officers ensuring approved products to patients encouraged to sanitise at entry.
Every touch point is a potential risk—or a chance to protect.
Related Posts
Topic Tags: Effective infection control is central to resident safety in aged care, where close living environments, chronic illness, and…
Topic Tags: In healthcare environments, many pathogens spread through high-touch surfaces that look clean but still carry organic residue. Traditional…
Topic Tags: Maintaining a safe, clean environment in aged care facilities is essential for protecting residents, supporting staff, and meeting…