Topic Tags:
What Do Hospitals Use to Clean?
Maintaining hygiene in hospitals is non-negotiable. Every surface, tool, and process must meet strict infection control standards to protect patients, staff, and visitors. In Australia, cleaning practices are guided by national infection prevention standards and regulated disinfectant requirements. Instead of relying on everyday cleaning products, hospitals use TGA-listed hospital-grade disinfectants, specialised tools, and personal protective equipment (PPE) to ensure every clean is safe and compliant.
3 Key Takeaways:
- Hospitals use TGA-listed hospital-grade disinfectants and neutral detergents to clean and disinfect surfaces, ensuring proven effectiveness against pathogens.
- Specialised tools and equipment like disposable cloths and mops, microfiber cloths, colour-coded mops, HEPA vacuums, and cleaning trolleys are used to reduce cross-contamination and improve cleaning outcomes.
- Proper storage of clean supplies and strict PPE use by cleaning staff are essential to maintaining Australian healthcare hygiene standards and protecting both patients and workers.
This guide explains the approved cleaning products, equipment, storage practices, and PPE requirements that underpin hospital cleaning in Australia.
Hospital-Grade Disinfectants and Standards
In Australia, hospital-grade disinfectants are required to comply with the TGA’s standards (such as Therapeutic Goods Order No.104, the Standard for Disinfectants and Sanitary Products) before they can be supplied and used in healthcare settings. Infection control guidelines recommend only using hospital-grade or chlorine-based disinfectants proven effective against healthcare-associated pathogens.
These products are applied after surfaces are cleaned with detergent, unless a combined detergent–disinfectant is used. To work effectively, factors like contact time, concentration, and surface suitability must always be followed.
Cleaning Tools and Equipment in Healthcare
Hospital environmental cleaning relies on a range of specialised tools and equipment designed to thoroughly clean surfaces while minimising infection risks. Common cleaning tools and practices include:
Dedicated Cleaning Cloths and Mops
Preferred for their effectiveness at removing microbes. They must be laundered daily or used as single-use disposables to prevent cross-contamination as per hospital laundry standards (e.g. AS/NZS 4146).
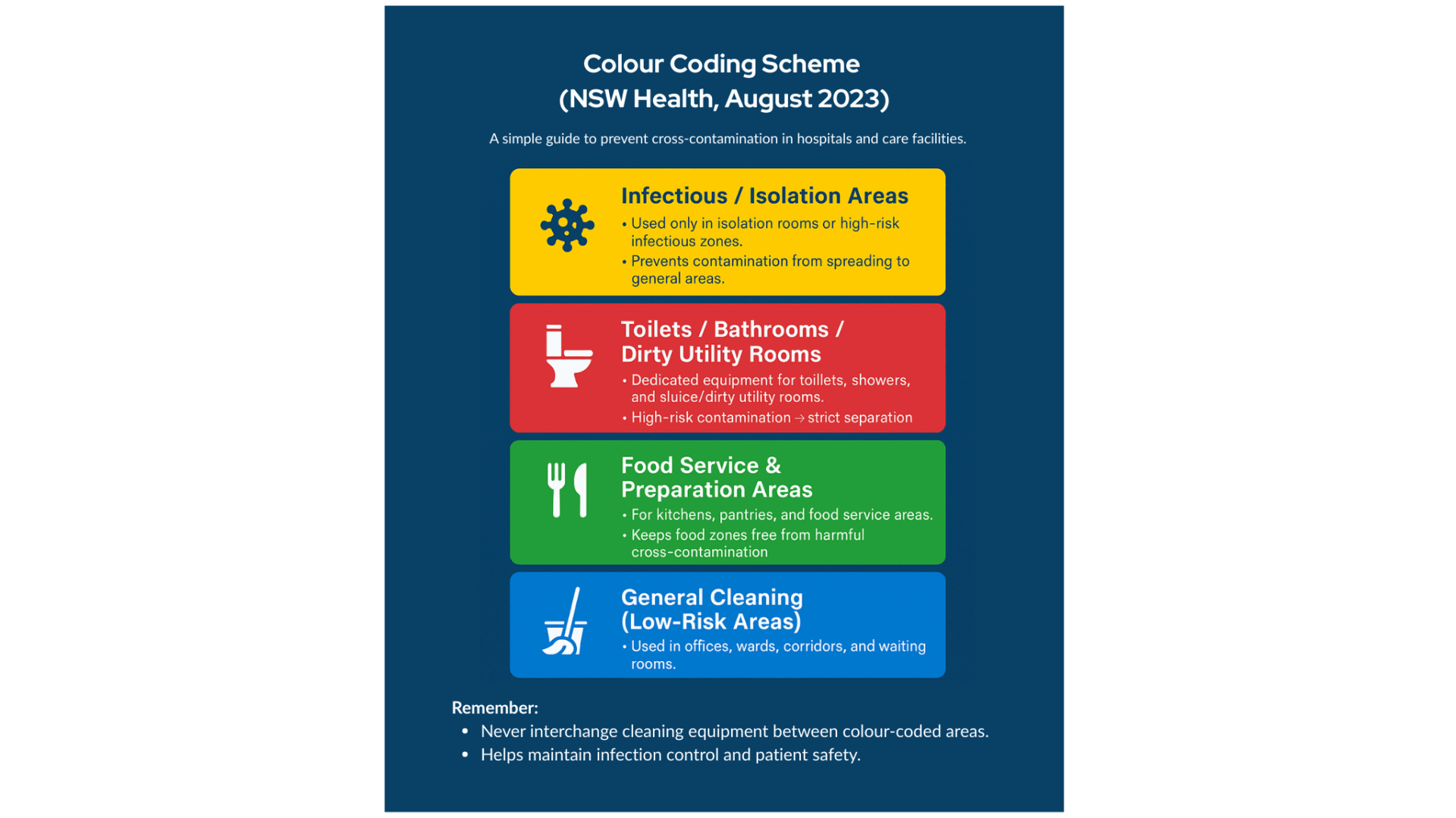
Colour-Coded Equipment
| Cloths, mops, and buckets are colour-coded for specific areas (e.g. bathrooms vs. food prep) to prevent cross-use and contamination. |
Cleaning Solutions and Buckets
Fresh detergent or detergent–disinfectant solutions are prepared daily. Two-bucket systems (one for detergent solution and one for rinsing the mop) or pre-moistened wipes avoid spreading germs with dirty water. Neutral detergents are generally used for routine surface cleaning, as most surfaces can be cleaned effectively with detergent and water alone. Disinfectant is added after cleaning only when needed (such as in isolation rooms or outbreaks), per risk assessment.
Cleaning Trolleys/Carts
Designed to separate clean and dirty items, with secure storage for chemicals and waste. Carts must be cleaned daily and never carry personal items. In some settings (e.g. aged care homes), carts are equipped with a locked compartment for disposed waste, and the cart should remain locked whenever it’s unattended to prevent unauthorised access to cleaning agents.
Vacuum Cleaners with HEPA Filters
Used on carpets (though discouraged in clinical areas) to trap dust and microbes. Infection control guidelines advise that if carpets are present in patient areas, they should be vacuumed daily with a well-maintained HEPA-filter vacuum to minimise dust and aerosolised pathogens. Spills require steam cleaning per Australian standards.
Storage of Clean Supplies and Equipment
Proper storage of clean supplies is essential to maintain their cleanliness and prevent contamination. Hospitals adhere to guidelines for storing items like clean linens, sterile supplies, and cleaning equipment:
Designated Clean Storage Areas
Clean linens, sterile instruments, and consumables are kept in clean, dry, covered spaces separate from soiled items. Cupboards and trolleys should remain closed when not in use.
Avoiding Contamination
Supplies must not be stored in soiled utility rooms, bathrooms, corridors, or on the floor. Stock rotation (“first in, first out”) prevents dust build-up and waste.
Housekeeping Rooms/Closets
Cleaning materials are stored in dedicated closets with sinks, ventilation, and secure cabinets for chemicals and PPE. These closets must not store food or personal items.
Maintenance of Cleaning Equipment
Mops, cloths, and buckets are cleaned, dried, and stored after each use. Reusables are laundered daily, and carts/closets left clean at the end of each shift to prevent contamination.
Personal Protective Equipment (PPE) for Cleaning Staff
Housekeeping and environmental services staff in hospitals must wear appropriate personal protective equipment to protect themselves and to prevent spreading contaminants during cleaning. The required PPE for cleaning workers is based on standard infection control precautions and the level of risk in the area they are cleaning:
Gloves
Single-use nitrile or vinyl gloves for all cleaning tasks, changed between areas or tasks. Always combined with hand hygiene before and after use.
Gowns or Aprons
Fluid-resistant aprons or disposable gowns protect clothing and skin when splashes are likely. Removed immediately after use to avoid cross-contamination.
Masks and Eye Protection
Surgical masks with goggles (or sometimes a P2/N95 respirator) or face shields protect against splashes, aerosols, or chemical sprays. The hospital ensures these PPE items meet relevant Australian Standards and are readily available to staff in all cleaning areas.
Respirators (P2/N95 masks)
Required for airborne precaution rooms (e.g. TB, measles). Staff must be fit-tested and trained, wearing a respirator plus gloves, gown, and eye protection.All PPE must be used correctly: staff receive training on how to put on and take off PPE in the proper sequence to avoid self-contamination. For example, gloves and apron/gown are removed (inside-out) before removing eye protection and mask, and the mask is removed last by its straps. After removing PPE, hand hygiene is performed immediately. Disposable PPE items (gloves, masks, etc.) are discarded safely. By wearing the required PPE and following these procedures, hospital cleaning personnel protect themselves and help maintain a hygienic, safe environment in compliance with infection control standards.

Partner with Namoli Healthcare for Trusted Hospital-Grade Cleaning
At Namoli Healthcare, we specialise exclusively in healthcare and hospital cleaning that meets Australia’s strictest hygiene standards.
Our teams are trained in infection control, use only TGA-listed hospital-grade disinfectants, and follow evidence-based protocols for every environment—from general wards to operating theatres.
With routine audits, clear compliance reporting, and tailored cleaning schedules, we help healthcare providers maintain safe, compliant, and hygienic facilities for patients, staff, and visitors.
Related Posts
Topic Tags: Sapovirus is a common cause of acute gastroenteritis, particularly in young children and aged‑care settings. Although symptoms are…
Topic Tags: Effective infection control is central to resident safety in aged care, where close living environments, chronic illness, and…
Topic Tags: In healthcare environments, many pathogens spread through high-touch surfaces that look clean but still carry organic residue. Traditional…